Welcome to John Theurer Cancer Center at Hackensack University Medical Center
A Leader in Cancer Care and Innovation
At the John Theurer Cancer Center, part of Hackensack University Medical Center and the Hackensack Meridian Health network, we are proud to be one of the most renowned cancer treatment centers in the United States. Recognized for our advanced technology, research excellence, and compassionate patient care, we offer comprehensive oncology services that are tailored to each individual.
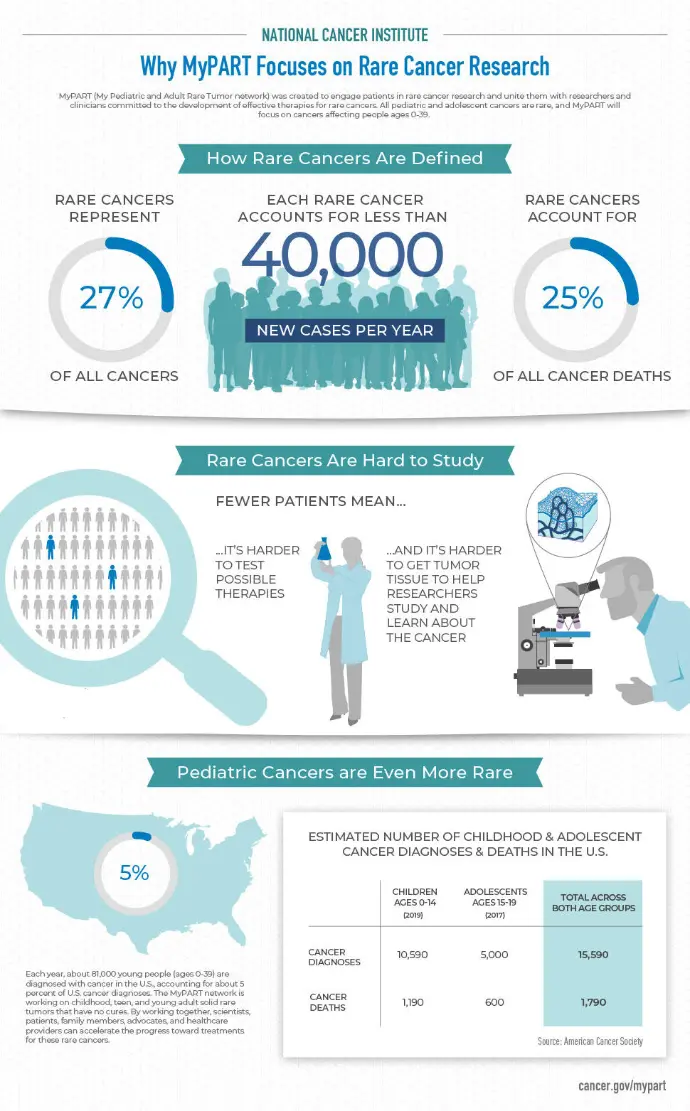
Whether you're seeking cutting-edge therapies, personalized cancer treatment, or access to clinical trials, our center remains at the forefront of cancer innovation, in collaboration with institutions like the National Cancer Institute (NCI) and the American Cancer Society.
What is Cancer?
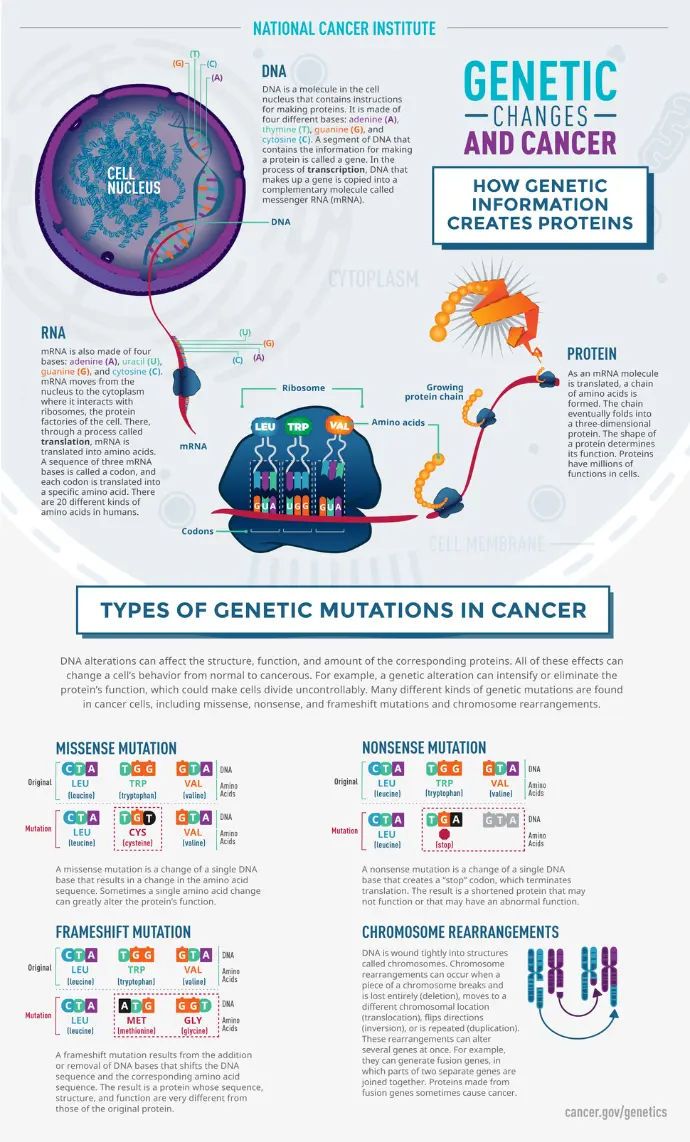
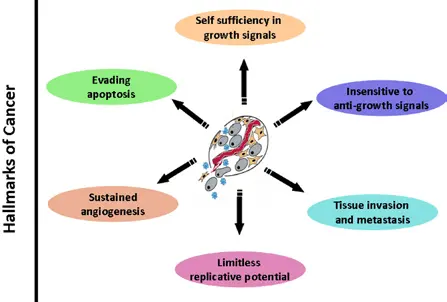
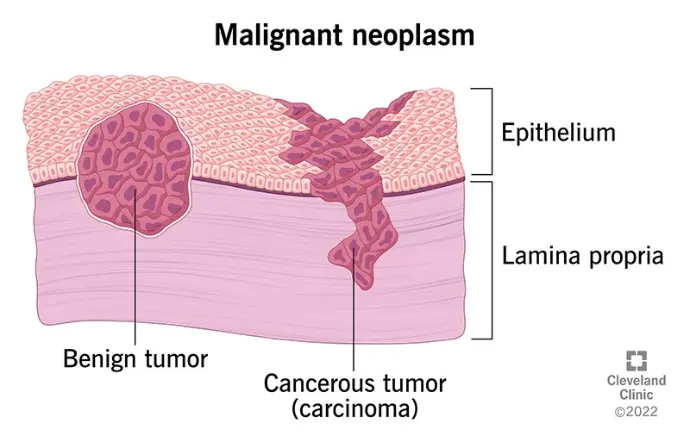
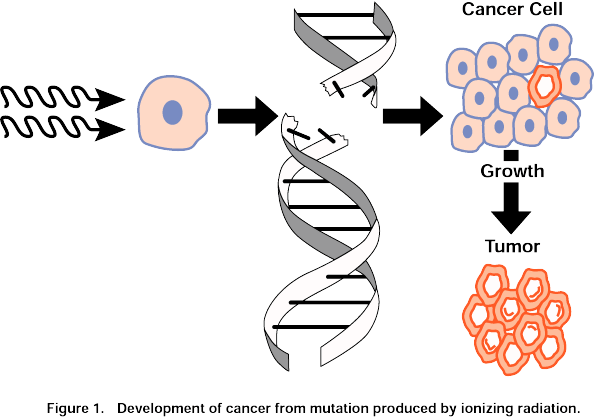
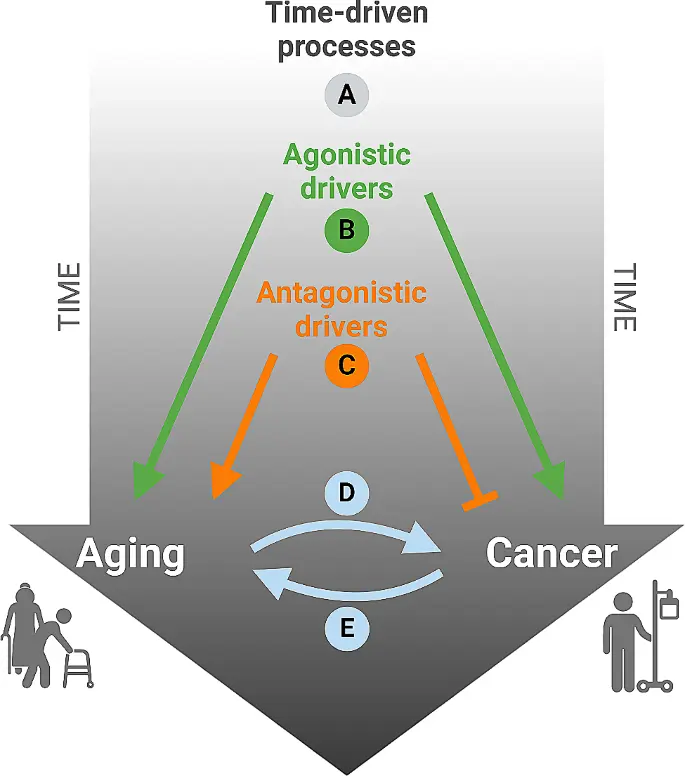
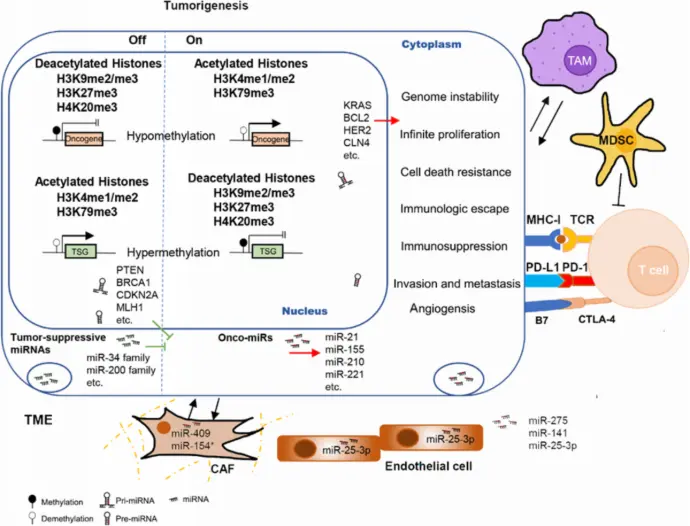
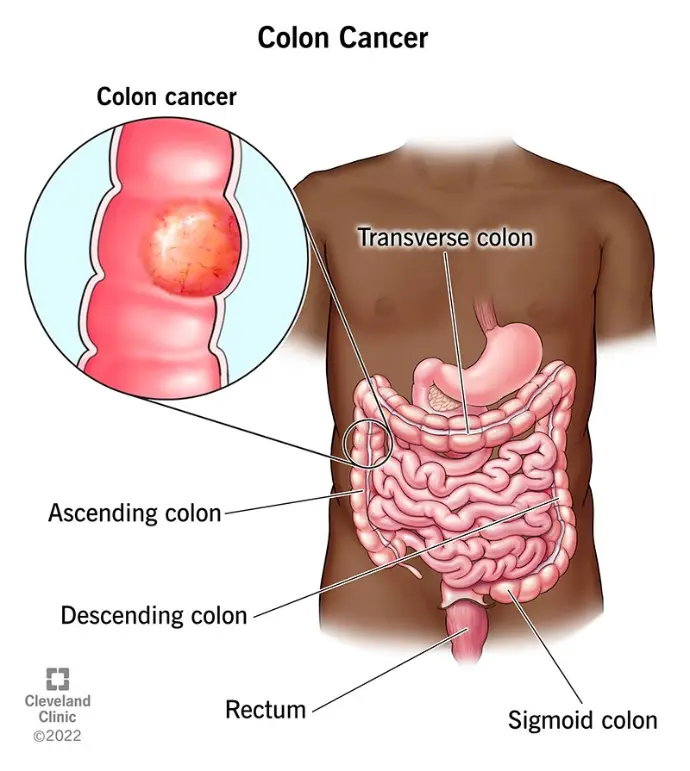
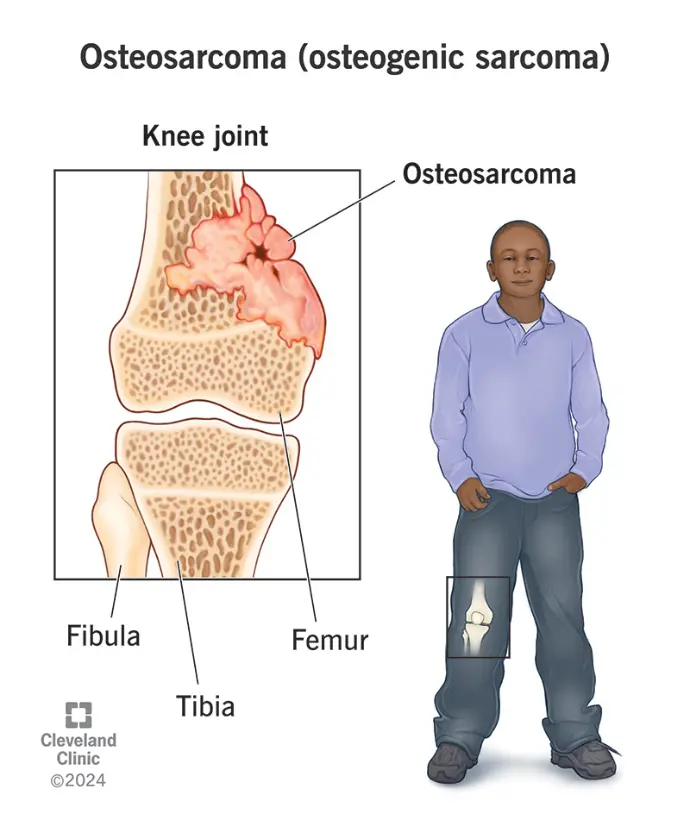
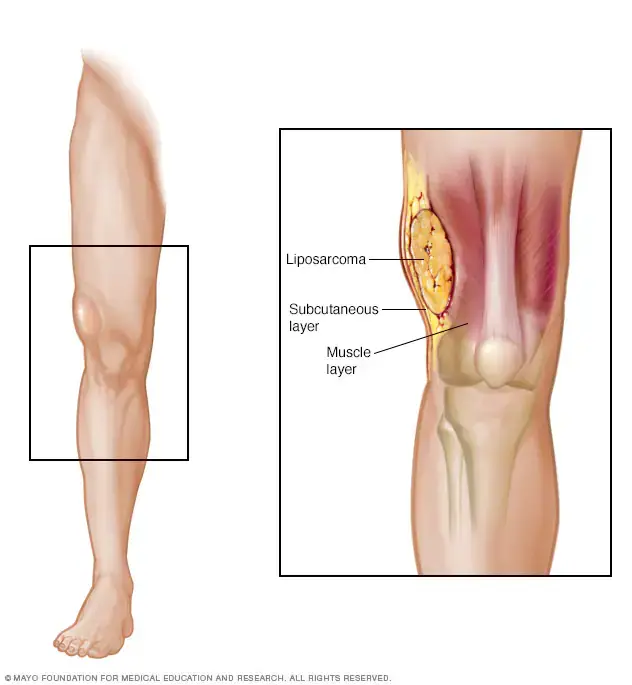
Cancer is not a single disease, but a group of related diseases characterized by the uncontrolled division of abnormal cells in the body. These cells can invade and destroy surrounding healthy tissue, and sometimes spread to other parts of the body through a process known as metastasis.
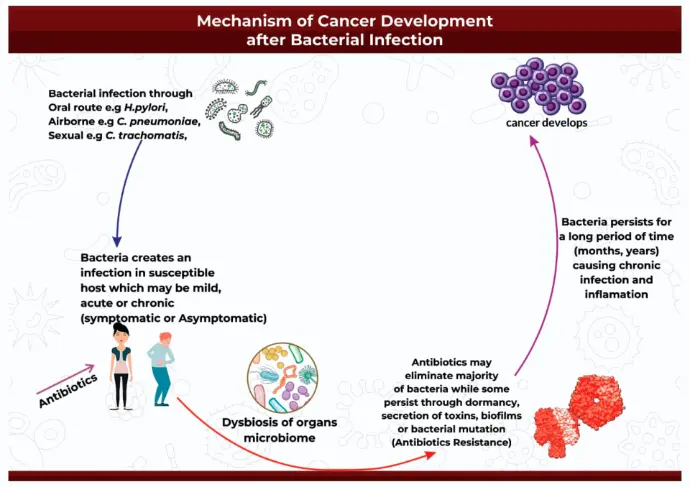
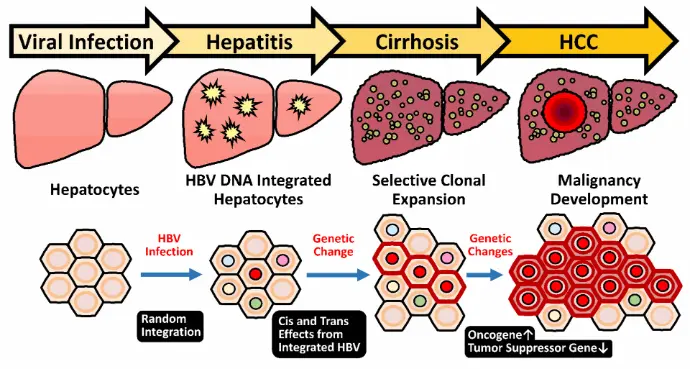
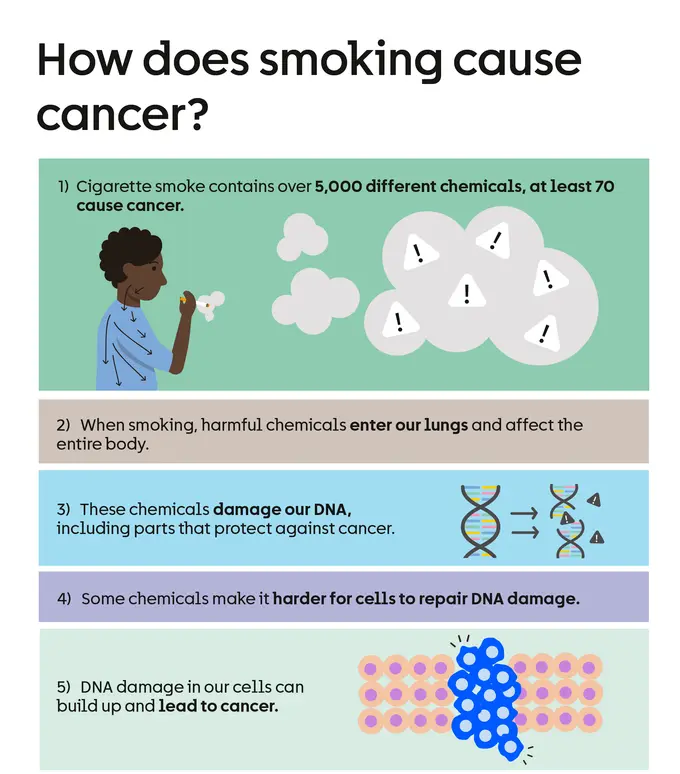
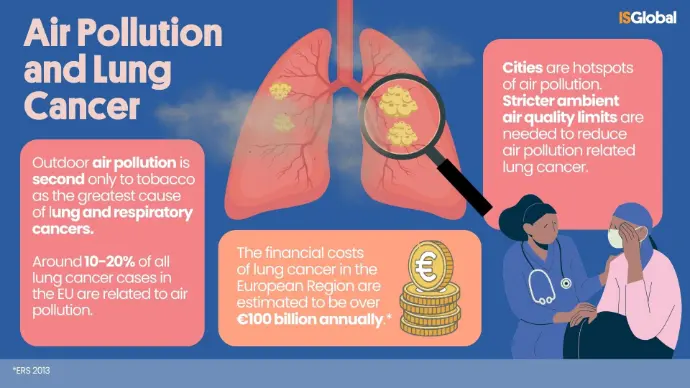
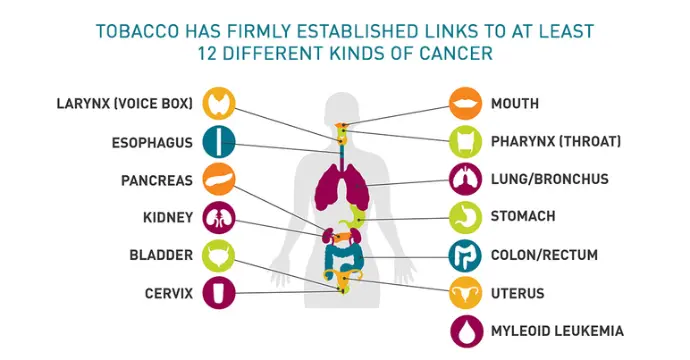
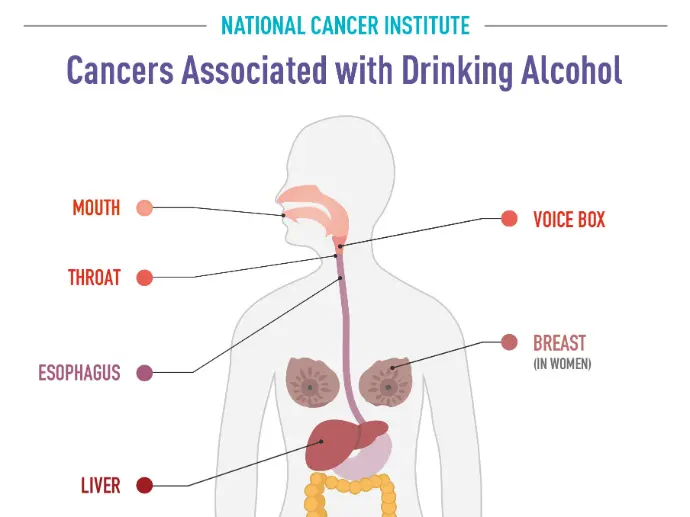
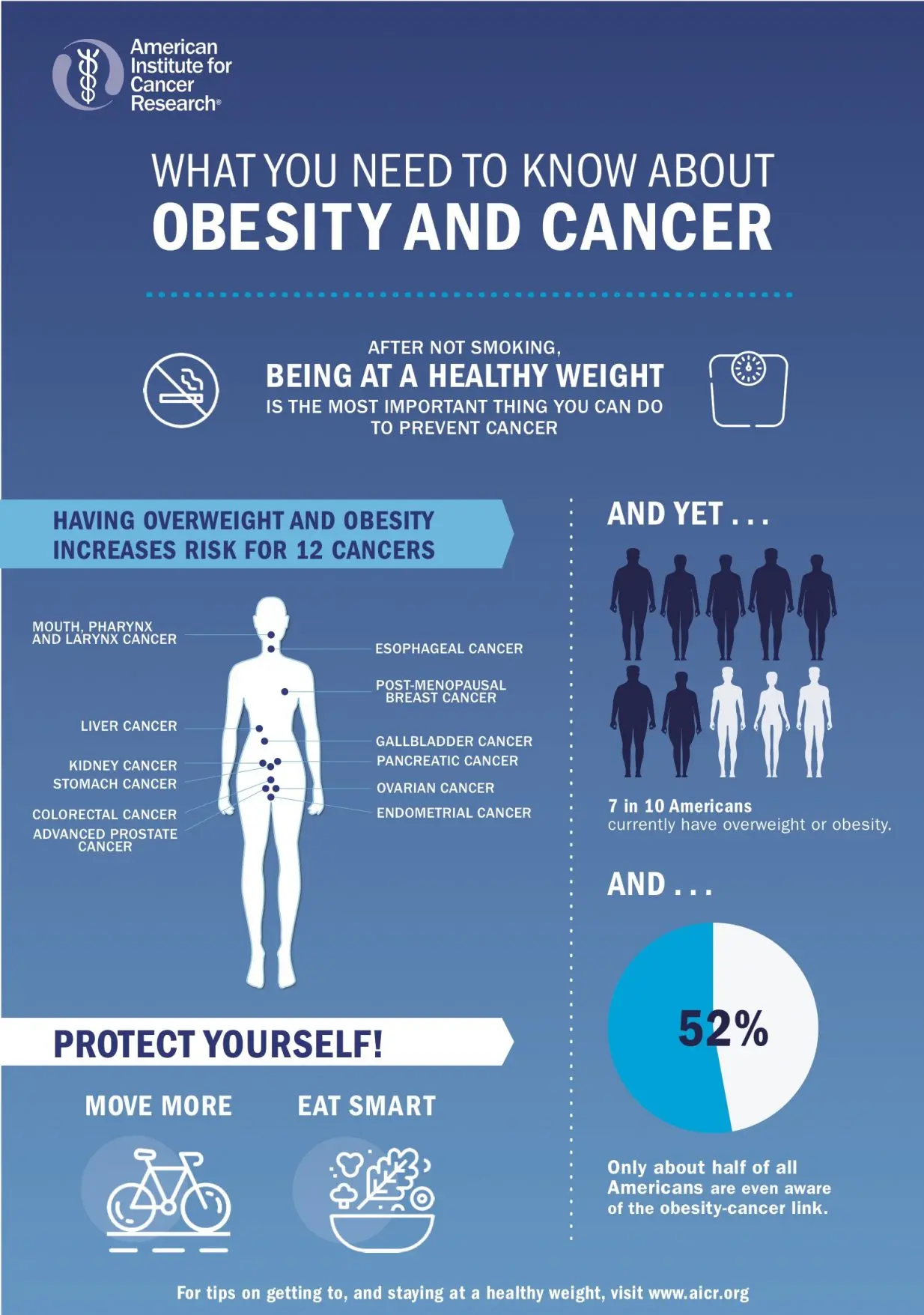
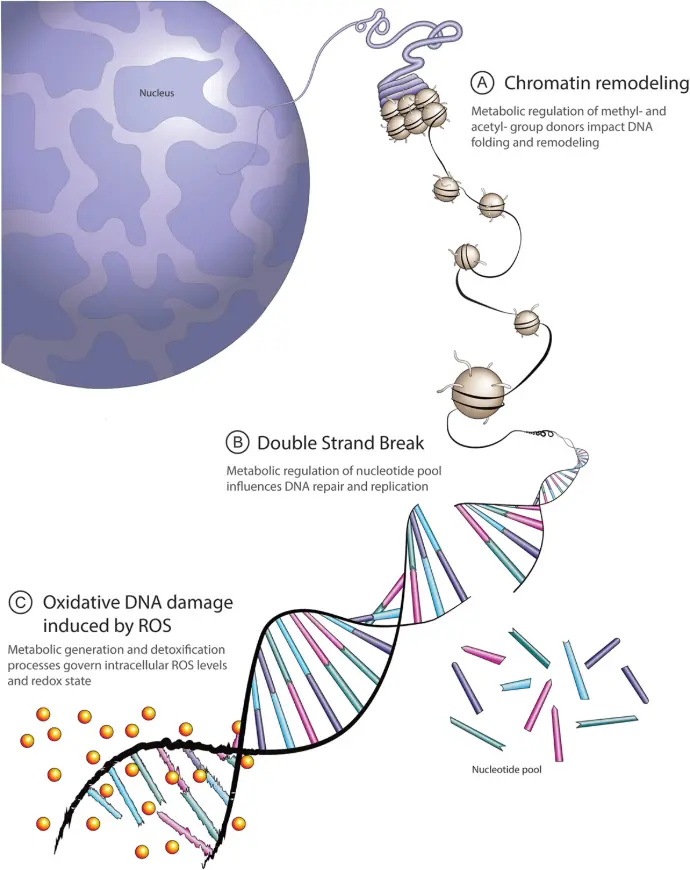
At its core, cancer begins with changes in the DNA within cells. These genetic mutations may be triggered by environmental factors (such as smoking, UV exposure, or chemicals), inherited genetic predispositions, or random errors during cell replication.
Cancer can develop in virtually any tissue or organ and can remain localized or become invasive and systemic.
Cancer symptoms vary depending on the type and location of the disease. However, some general signs to watch for include:
- Unexplained weight loss
- Persistent fatigue
- Lumps or masses that can be felt through the skin
- Changes in skin (darkening, yellowing, redness)
- Changes in bowel or bladder habits
- Difficulty swallowing or persistent indigestion
- Chronic cough or hoarseness
- Unusual bleeding or discharge
Early detection significantly improves treatment outcomes. Therefore, recognizing and acting on these symptoms is crucial.
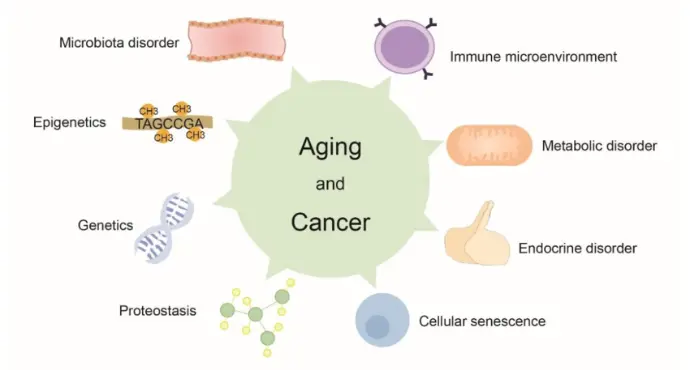
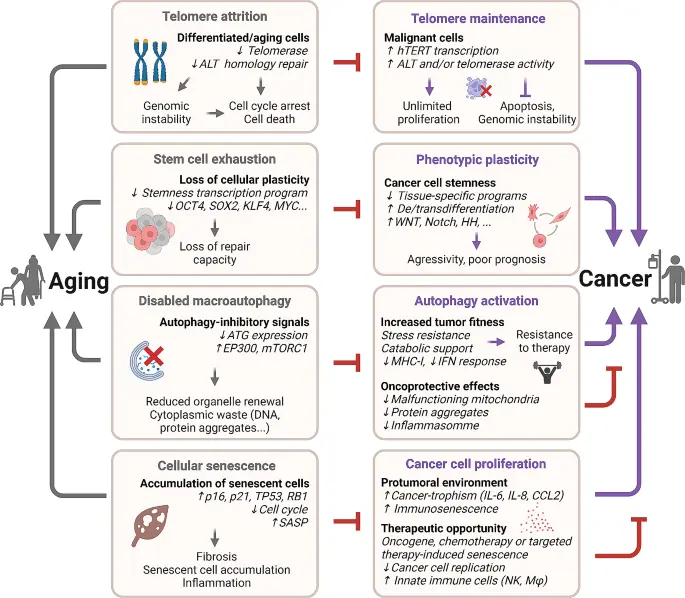
Cancer is not caused by a single factor, but by a complex interaction of genetic, environmental, and lifestyle elements. Understanding the root causes of cancer is essential for prevention, early detection, and treatment. At leading institutions like the John Theurer Cancer Center at Hackensack University Medical Center, cutting-edge research continues to explore how these various factors contribute to the onset and progression of cancer.
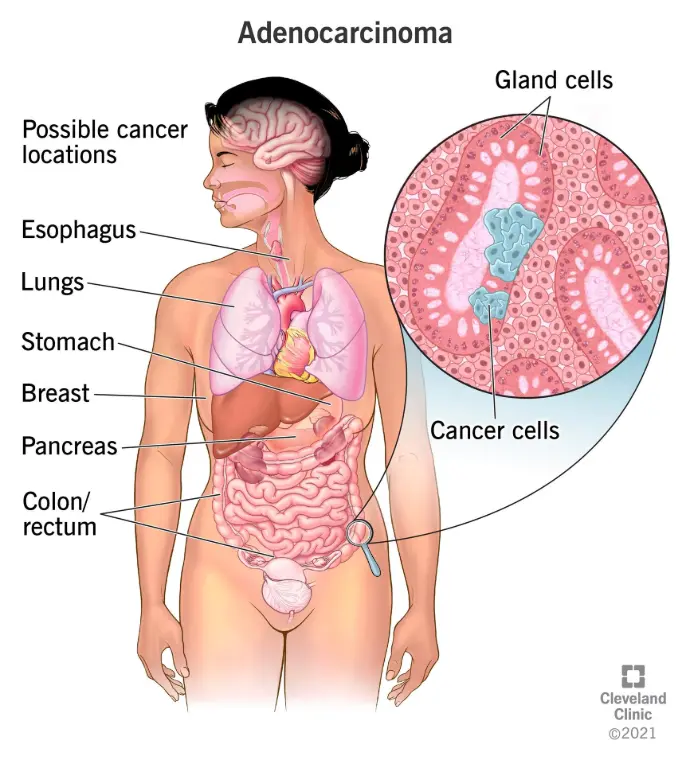
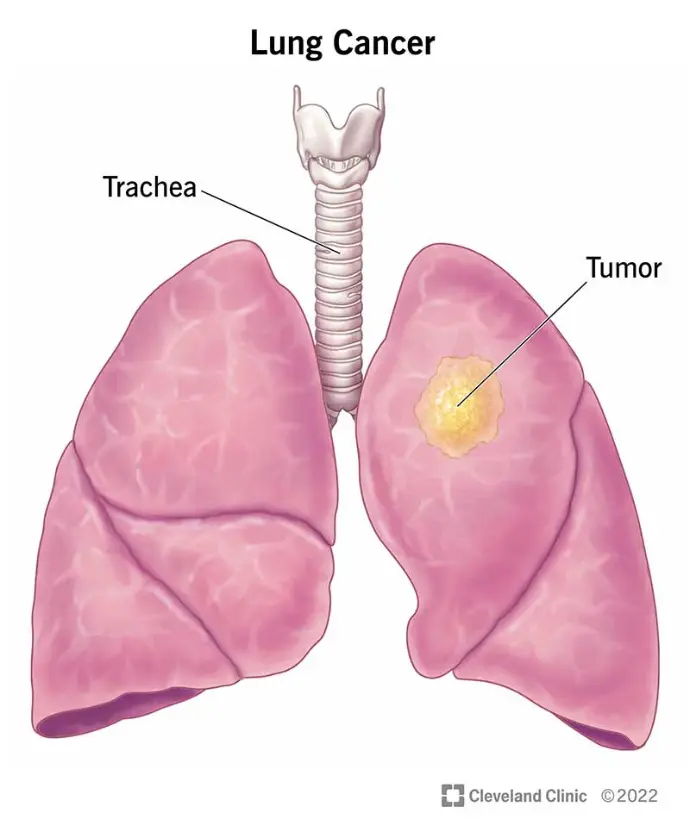
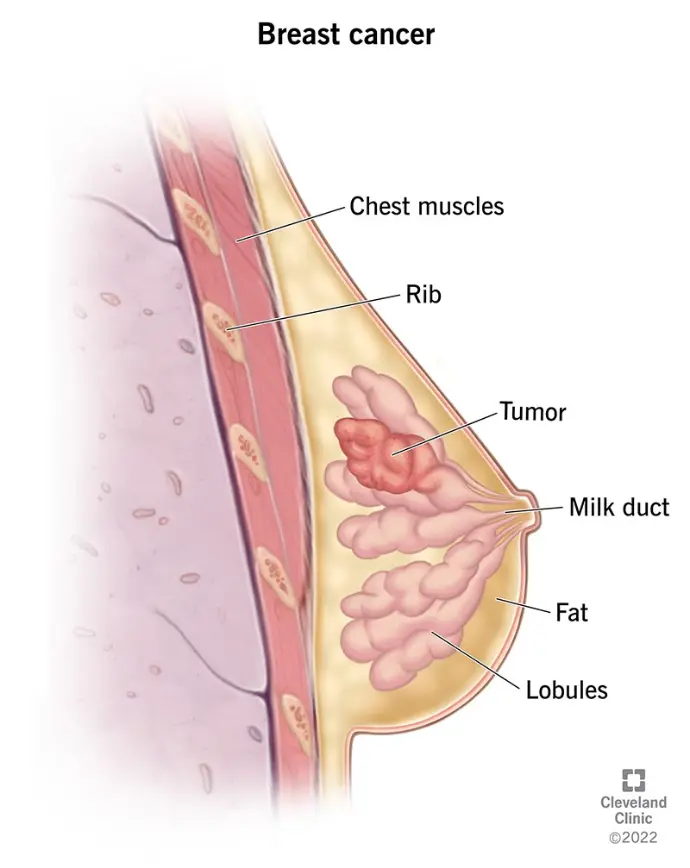
Types of Cancer
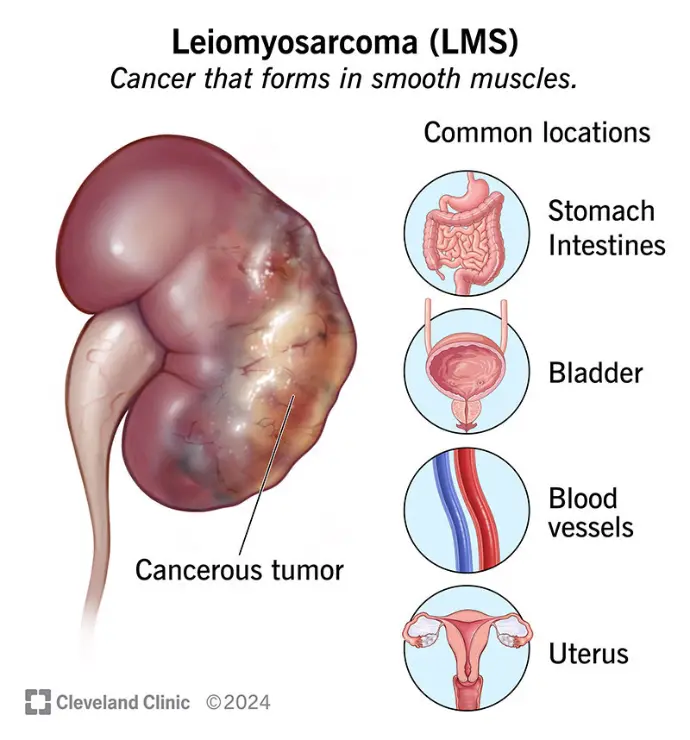
Cancer is not a single disease but a collection of over 100 distinct diseases, each classified based on the organ, tissue, or cell type from which it originates. Understanding these categories helps in selecting the most effective treatment approach and improving patient outcomes.
Below are the main types of cancer, categorized by the affected tissue or cell origin:
Cancer Diagnosis:
Tools and Techniques
From Physical Exams to Advanced Molecular Technologies
Diagnosing cancer accurately and at the earliest possible stage is crucial for successful treatment and improved survival rates. Today, medical science offers a wide range of diagnostic tools from basic clinical exams to cutting-edge molecular biology techniques. Here's a detailed overview of the major tools used to detect, confirm, and classify cancer.
A cancer diagnosis often begins with a routine physical exam, where the doctor checks for:
- Unusual lumps or masses
- Changes in the skin (moles or lesions)
- Abnormal swelling in lymph nodes
- Pain, fatigue, or unexpected weight loss
While not sufficient for a definitive diagnosis, this first step often leads to further testing when suspicion arises.
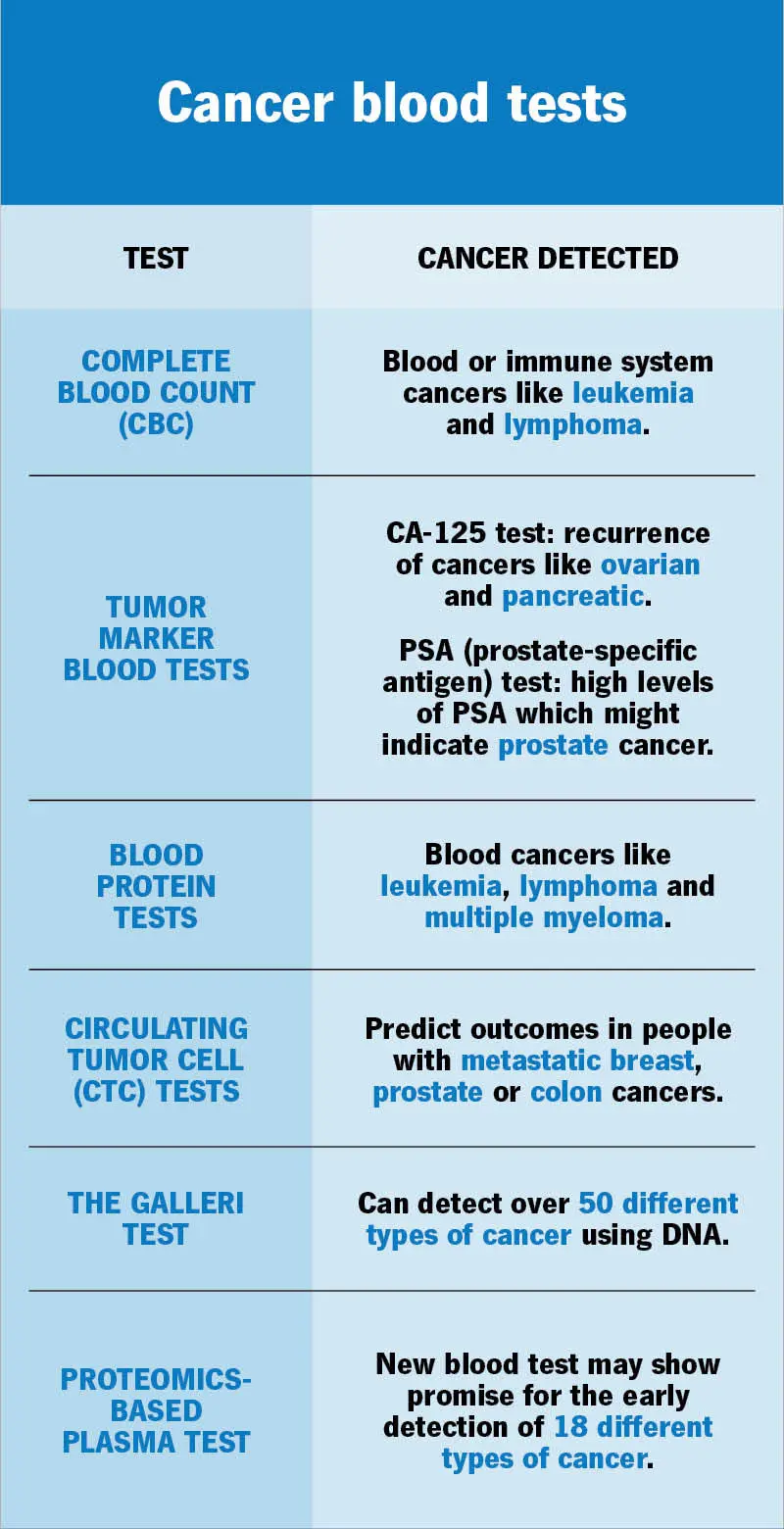
These tests help evaluate how the body is functioning and whether there are substances that could indicate cancer.
Blood Tests

- Tumor markers like PSA (prostate), CA-125 (ovarian), or AFP (liver)Read more
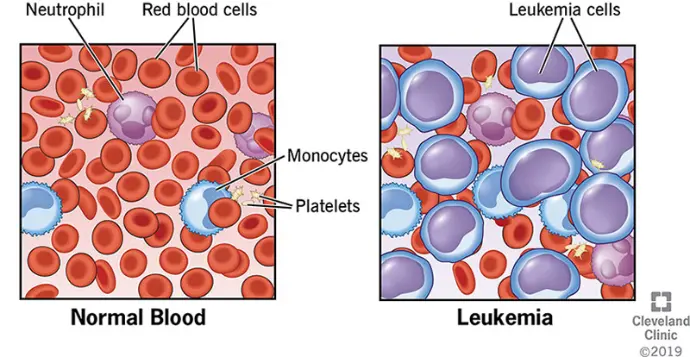
- Complete blood count (CBC) for blood cancers like leukemiaRead more
Urine and Other Fluids
May reveal abnormal protein levels or cell fragments

Histopathology

- The study of cells and tissues under the microscope after staining
- Can detect abnormal or cancerous cell structures
Imaging Techniques
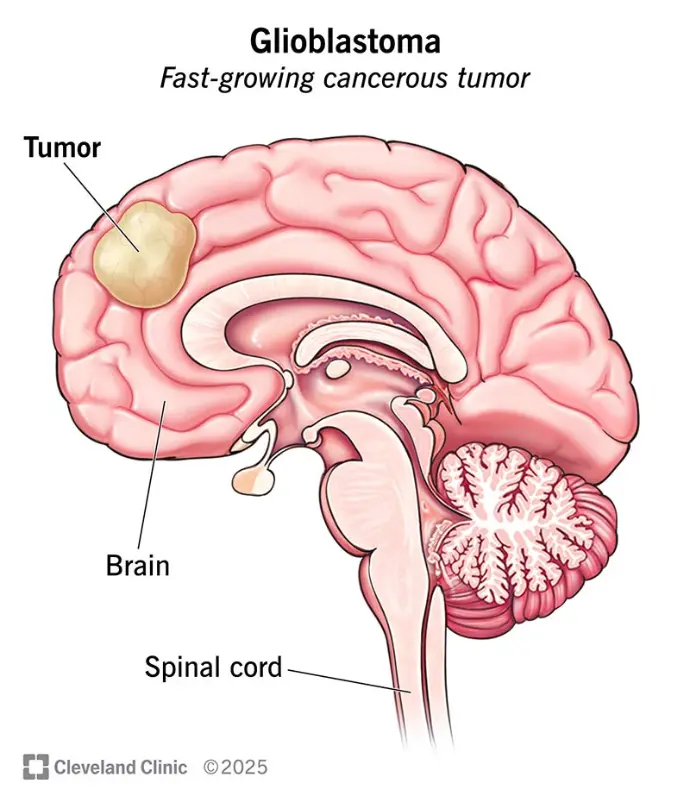
Modern imaging helps to detect tumors, define their size, and determine their location or spread.
Common Imaging Methods:
X-rays: First-line tool to detect large masses or bone metastases Read more

CT (Computed Tomography): Detailed cross-sectional imaging
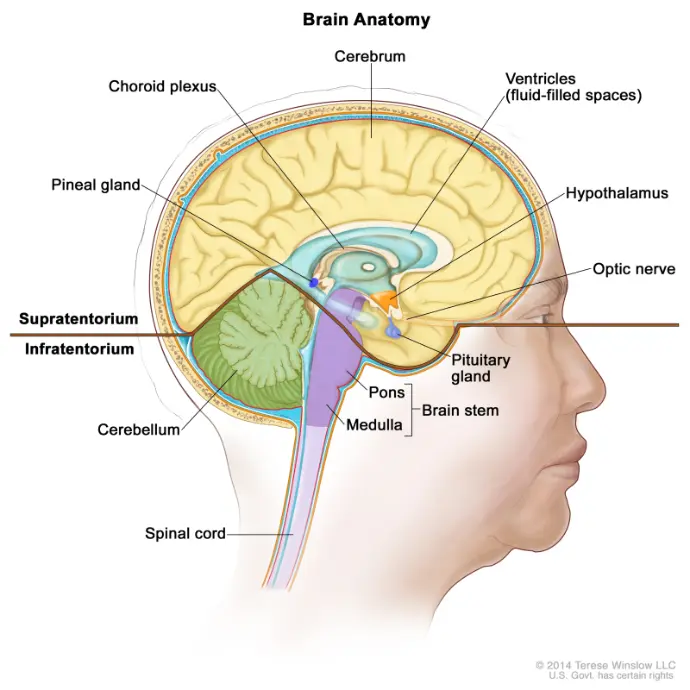
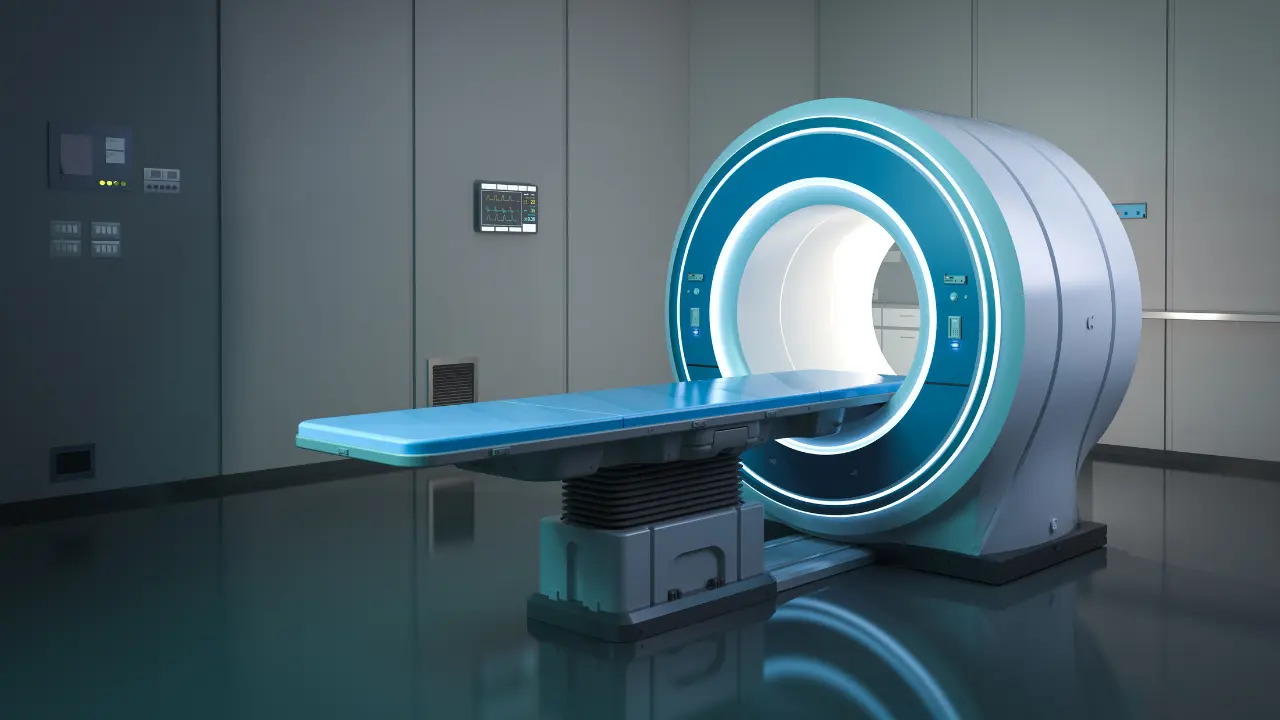
MRI (Magnetic Resonance Imaging): Excellent for soft tissues like the brain, spine, and muscles
Ultrasound: Non-invasive, used often in breast, thyroid, and pelvic imaging

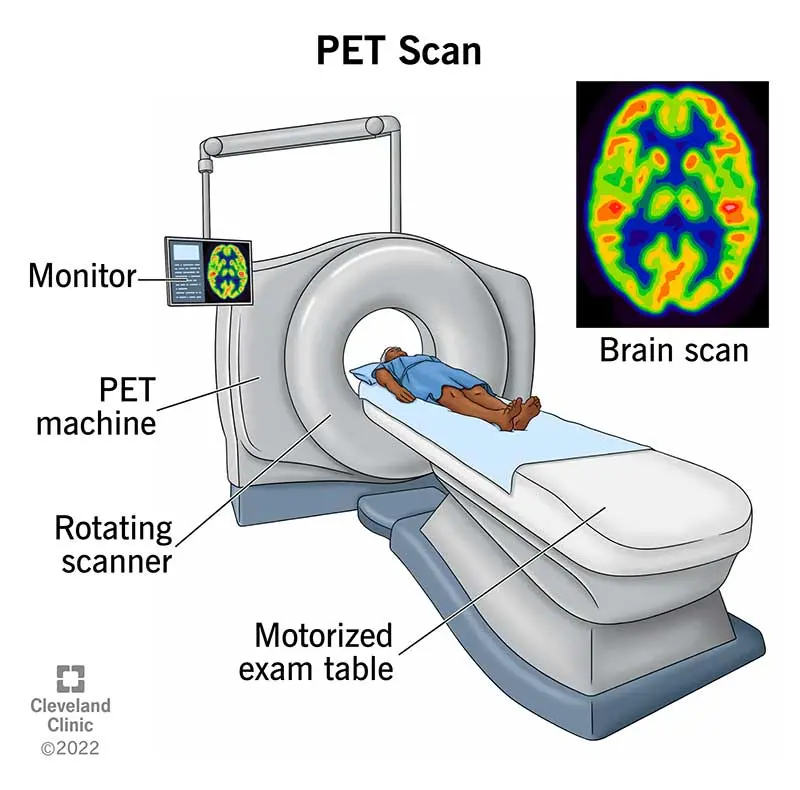
PET scans (Positron Emission Tomography): Highlights areas of high metabolic activity, often used to detect metastasis
These tools are often combined to provide a full picture of the cancer’s status and spread (staging).
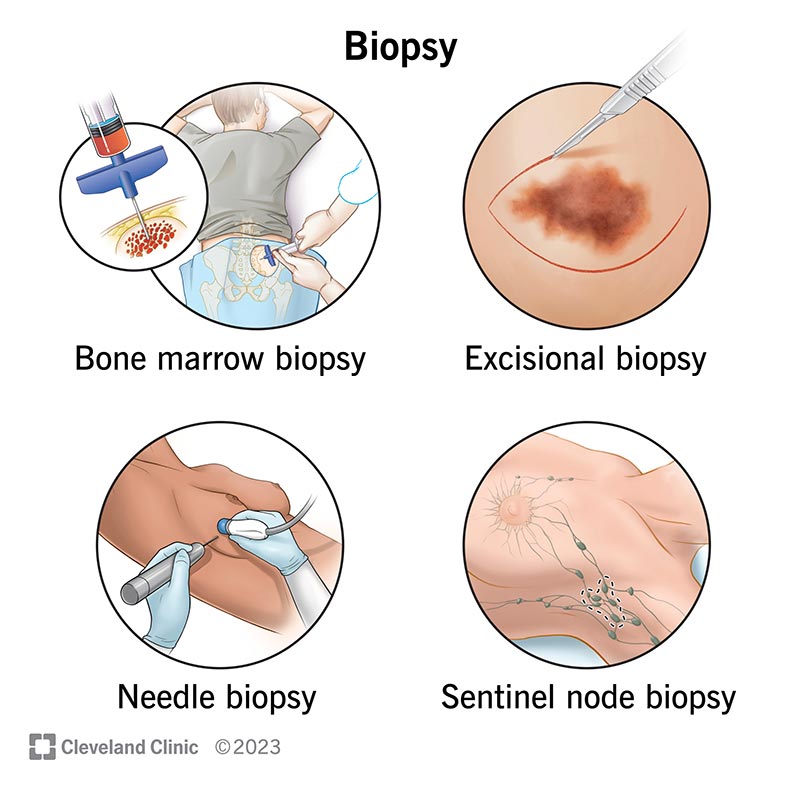
Biopsy:
The Gold Standard
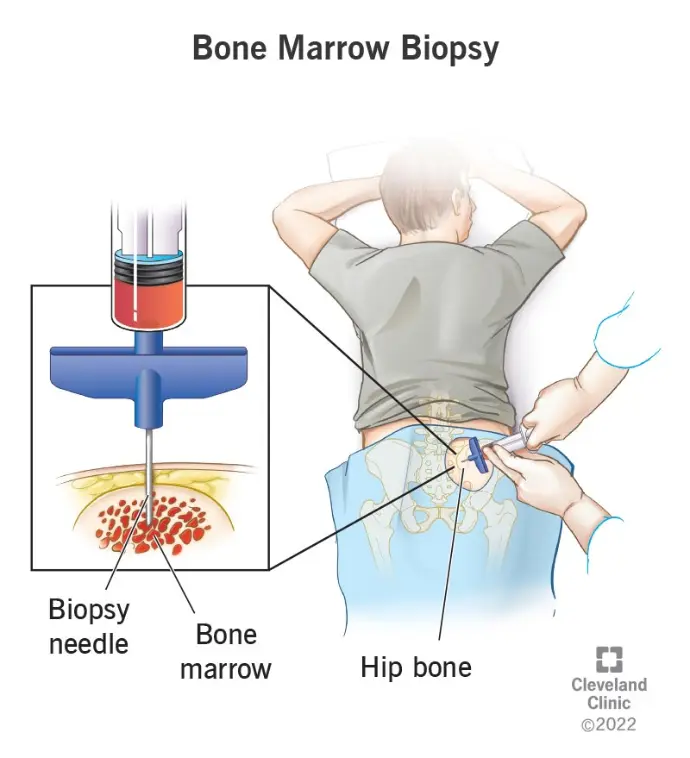
A biopsy involves collecting a sample of tissue from the suspected tumor and analyzing it under a microscope. It provides the most definitive diagnosis of cancer.
Types of Biopsies:
- Fine-needle aspiration
- Core needle biopsy
- Excisional biopsy (removal of the entire mass)
- Endoscopic biopsy (from internal organs via scopes)
The tissue is analyzed to determine:
- Cancer type
- Grade (how aggressive it is)
- Stage (extent of spread)
- Presence of hormone receptors or specific proteins (for targeted therapy decisions)
Genetic and Molecular Testing
Modern oncology relies heavily on molecular techniques to detect and understand cancer on a genetic level. These tools allow:
- Early detection (even before symptoms)
- Classification of cancer subtypes
- Tailoring of personalized therapies
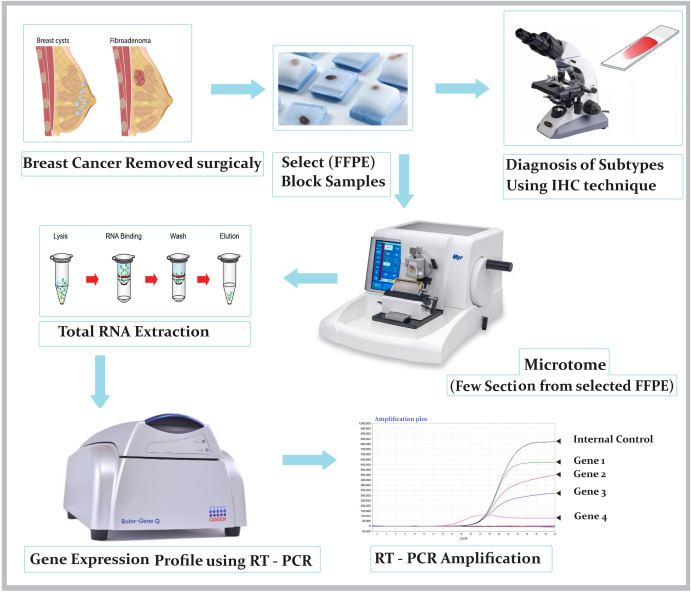
🔹 PCR (Polymerase Chain Reaction)
-
Amplifies small amounts of DNA/RNA to detect specific gene mutations, such as:
- BRCA1/2 (breast/ovarian cancer)
- KRAS, EGFR, BRAF (colorectal, lung, and melanoma)
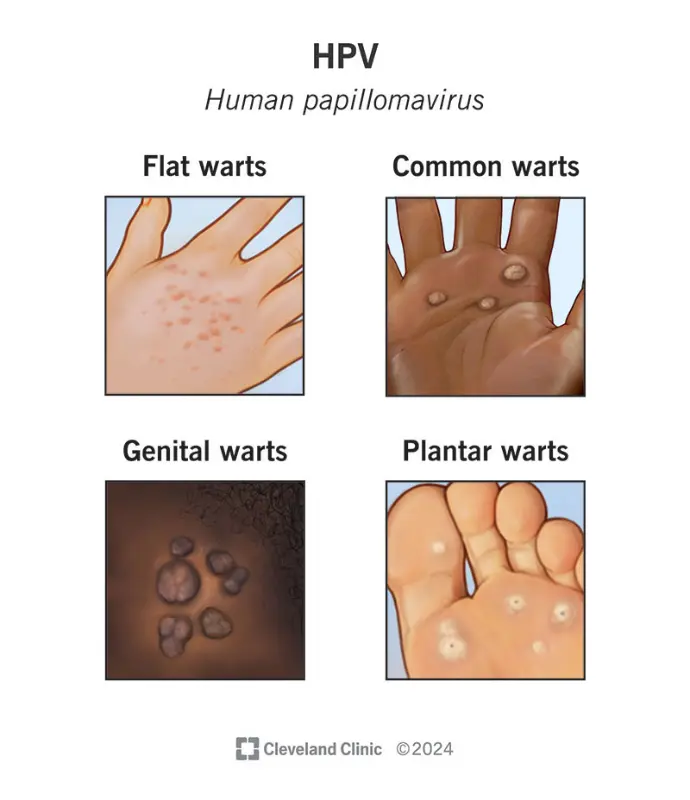
- Used in detecting viral oncogenes like HPV or HBV
🔹 RT-PCR (Reverse Transcriptase PCR)
- Used to detect gene expression levels or viral RNA (e.g., HPV or EBV in tumors)
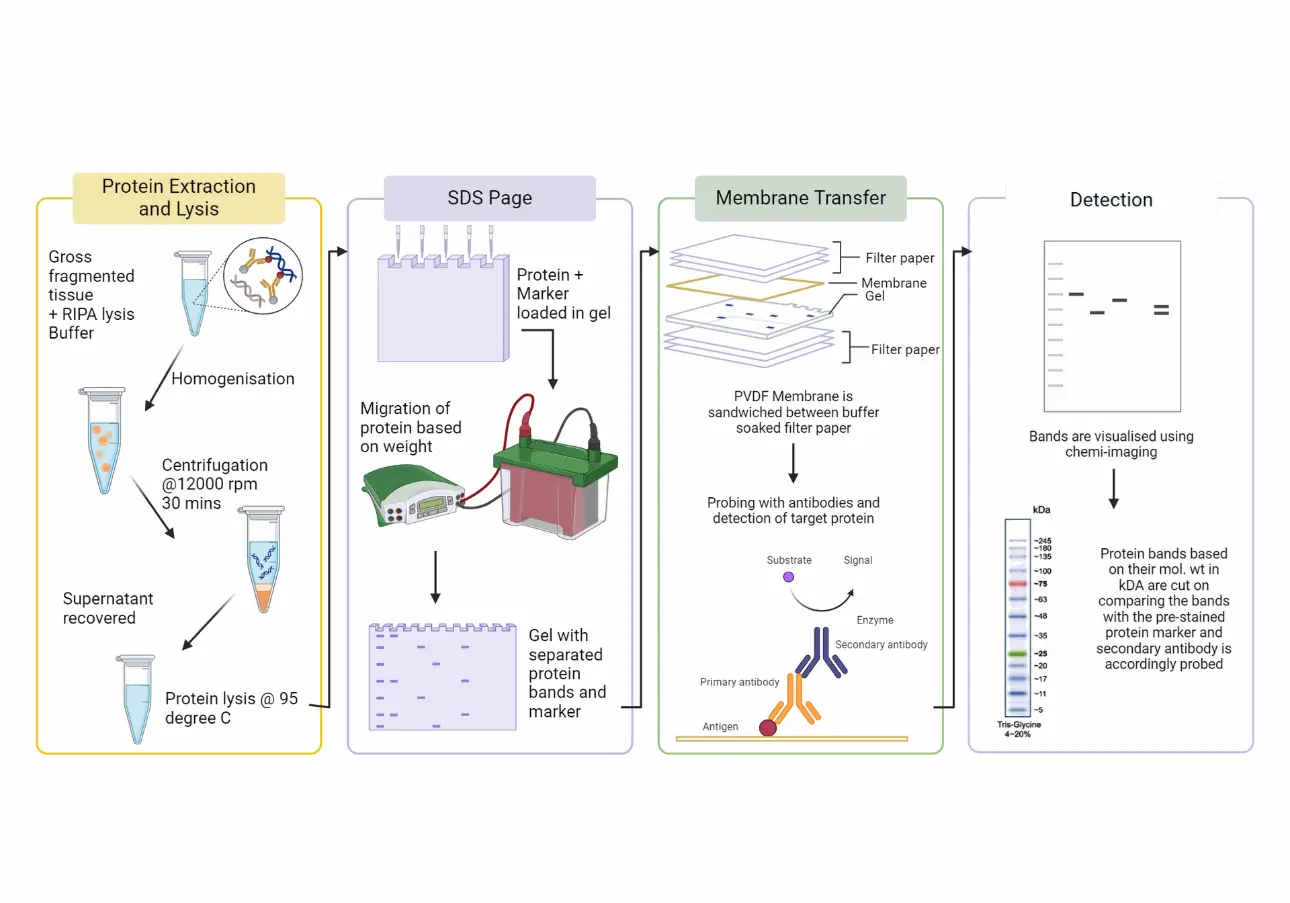
🔹 Western Blot
- Detects specific proteins in a tissue or blood sample
- Confirms presence or absence of tumor-related antigens or receptors
- Often used alongside ELISA to validate protein expression
- Useful for cancers involving abnormal protein signaling pathways
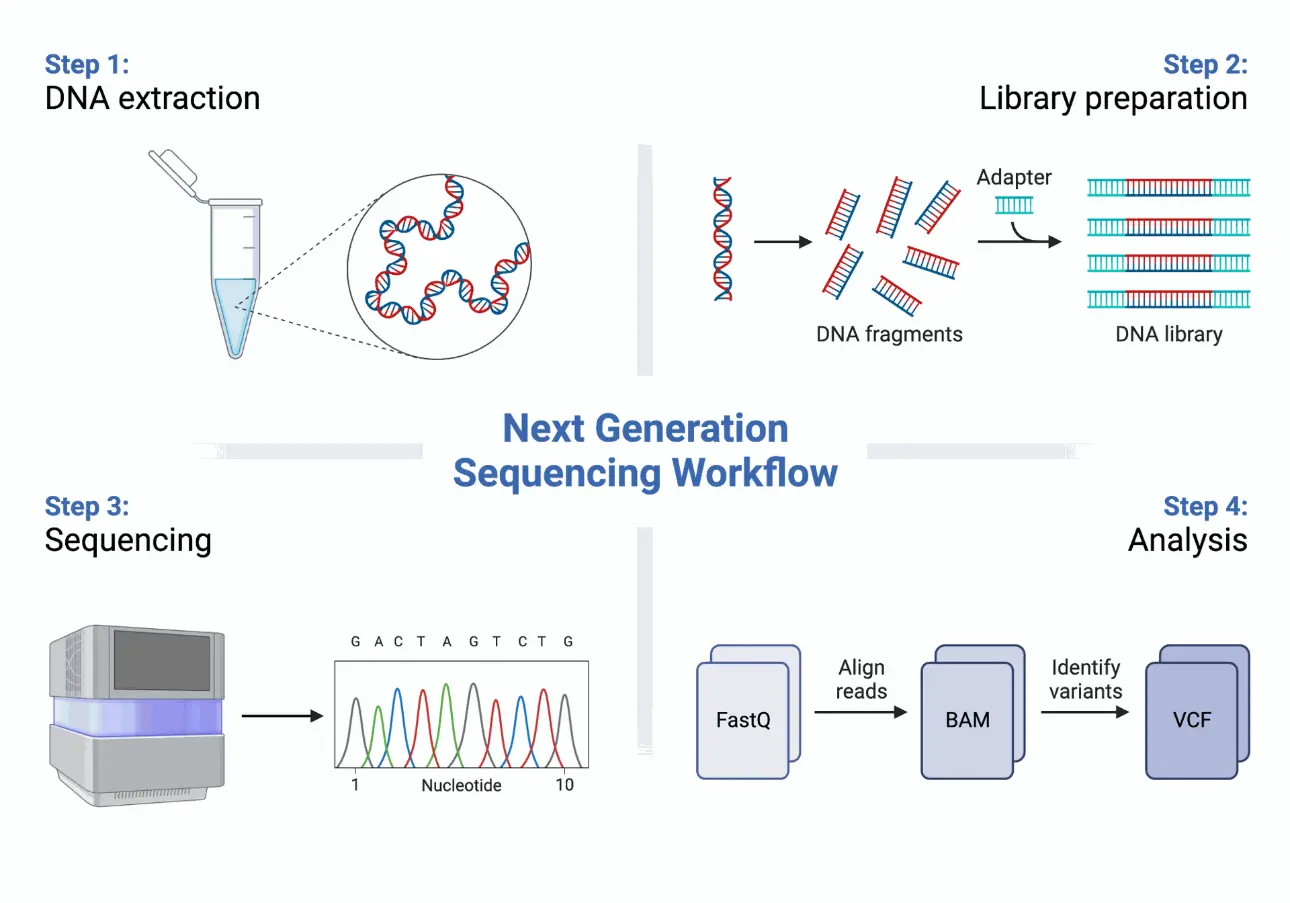
🔹 Next-Generation Sequencing (NGS) Read more
- Offers a full genomic profile of a tumor
- Detects hundreds of mutations at once
- Essential in precision oncology to guide immunotherapy and targeted treatments
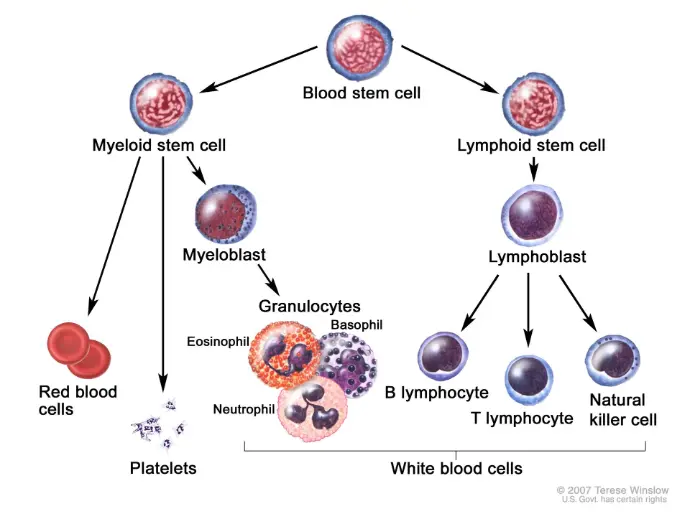
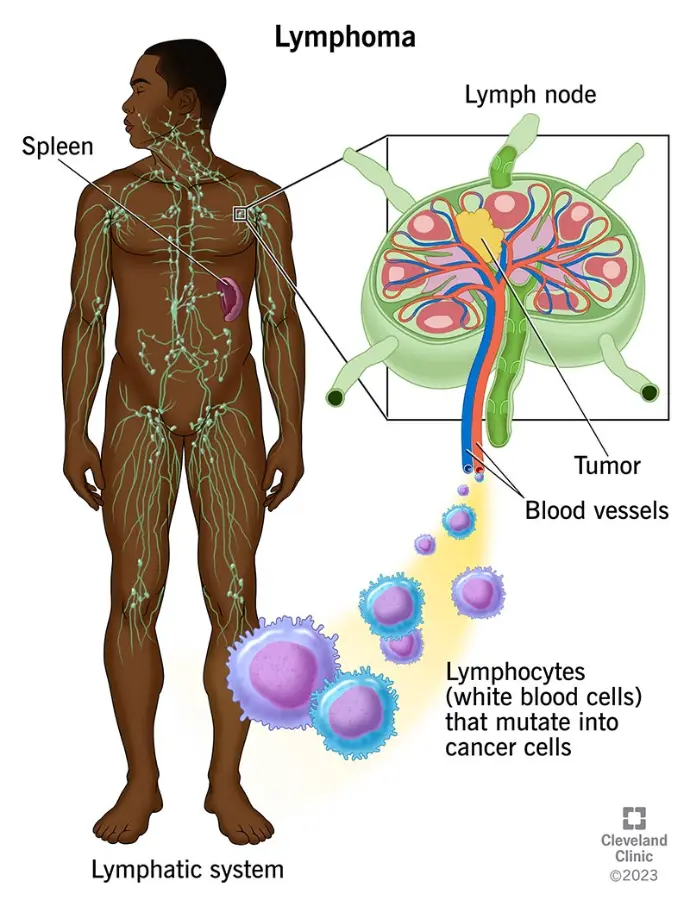
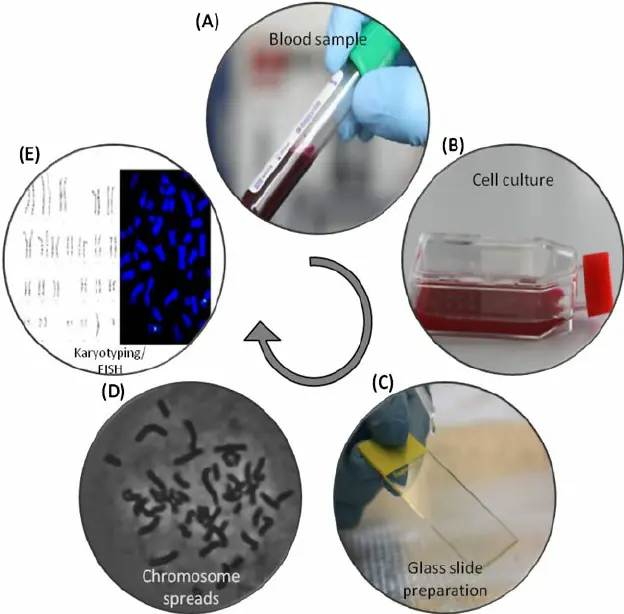
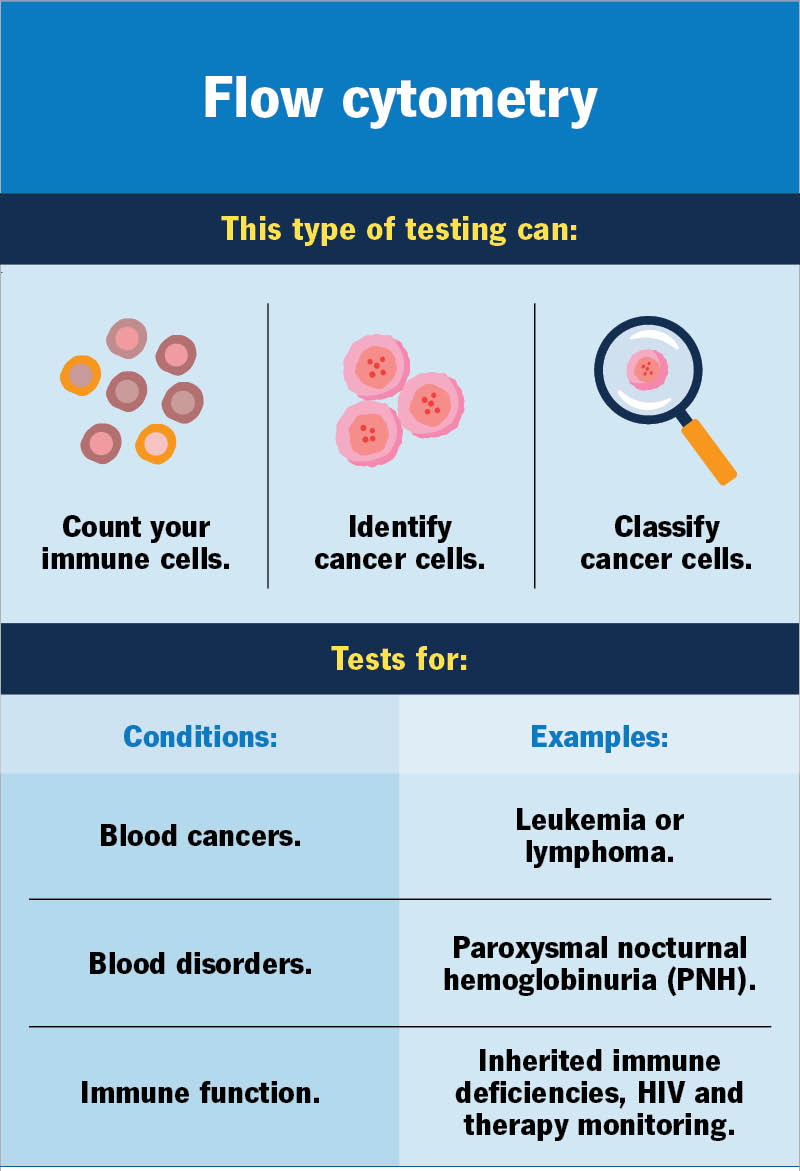
Cytogenetic and Flow Cytometry Testing
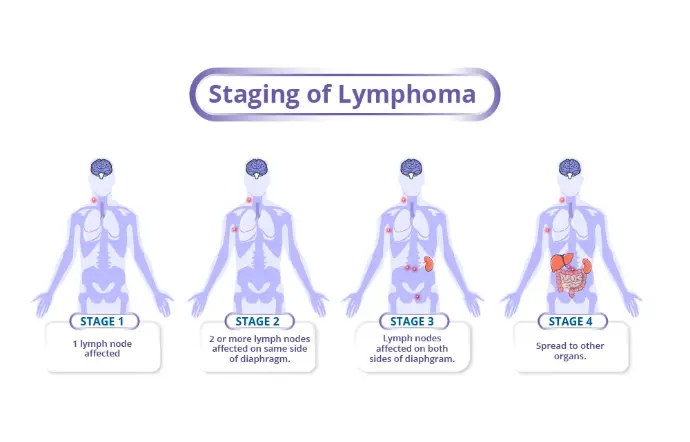
These are especially important in hematologic cancers like leukemia or lymphoma.
- Cytogenetics: Analyzes chromosomes for large-scale abnormalities (e.g., Philadelphia chromosome in CML)Read more
- Flow Cytometry: Measures cell size, shape, surface proteins; used in leukemia/lymphoma diagnosis and monitoringRead more
Liquid Biopsy (Emerging Tool)
A non-invasive test that detects circulating tumor DNA (ctDNA) or cancer cells in blood. Useful for:
Useful for:
- Monitoring cancer progression
- Detecting minimal residual disease
- Screening in high-risk individuals
Treatment Options
Cancer treatment is personalized and depends on the type, stage, and overall health of the patient.
Common treatment modalities include:
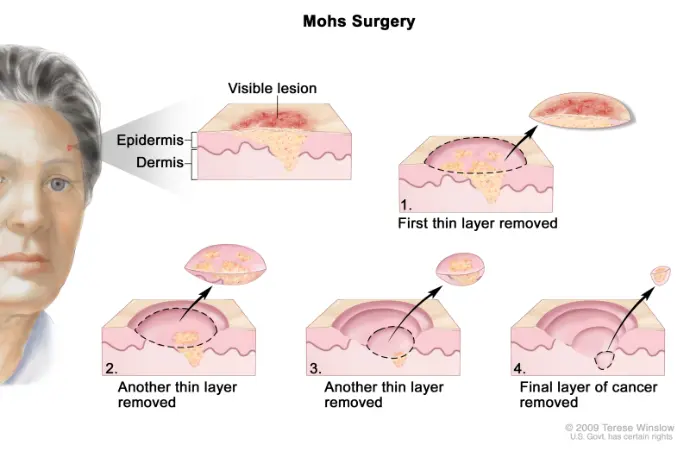
- Surgery : Removal of the tumor and surrounding tissue.
- Chemotherapy : Use of drugs to kill or inhibit cancer cell growth.
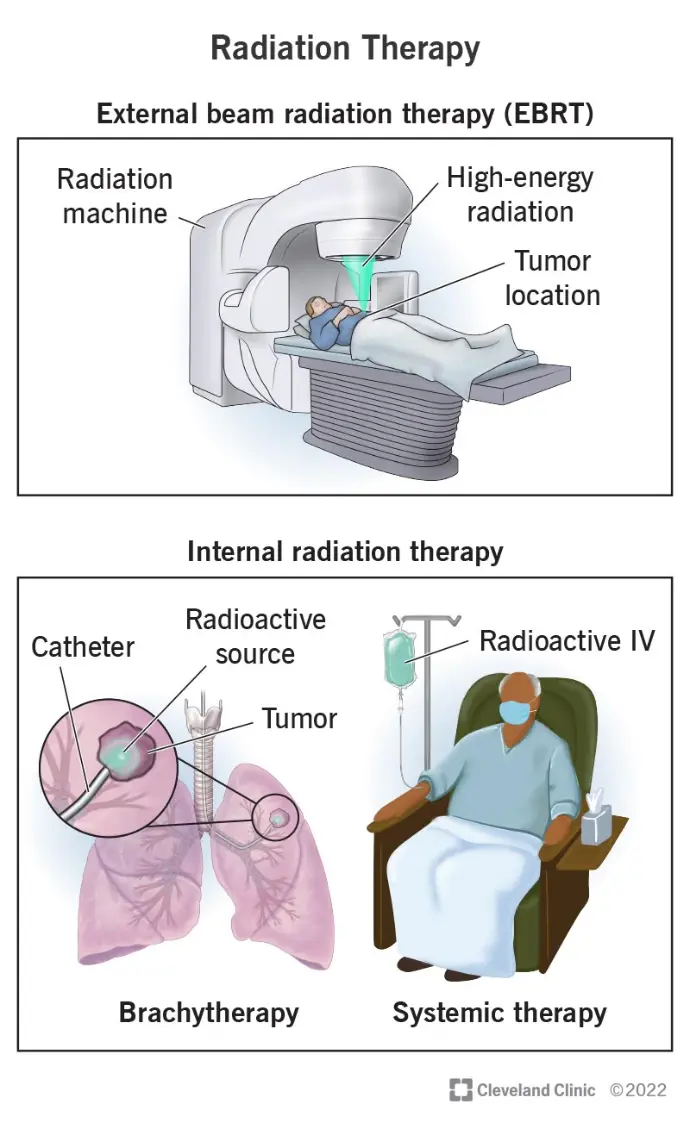
- Radiation Therapy : High-energy rays targeting cancer cells.
- Immunotherapy : Boosting the immune system to fight cancer.
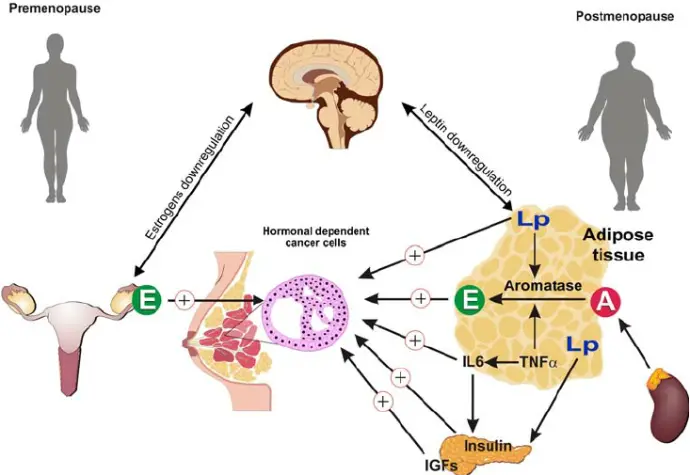
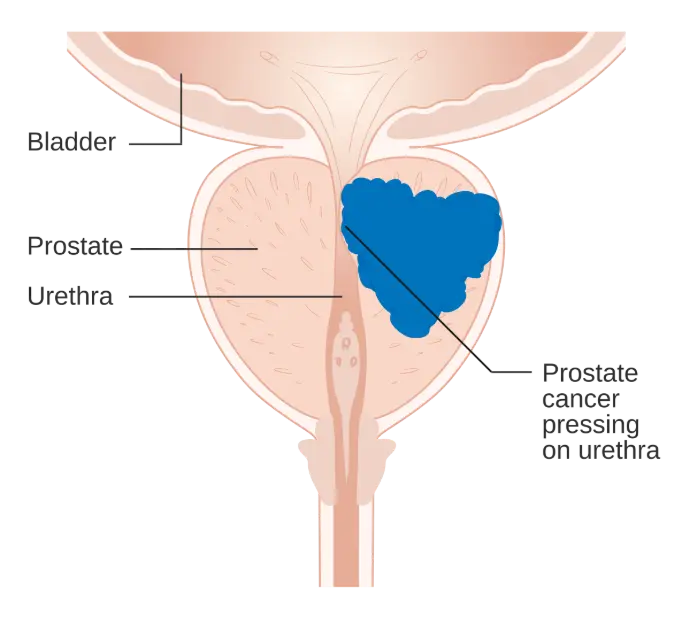
- Hormone Therapy : Especially in breast and prostate cancers.
- Targeted Therapy : Drugs that specifically target cancer cell molecules.
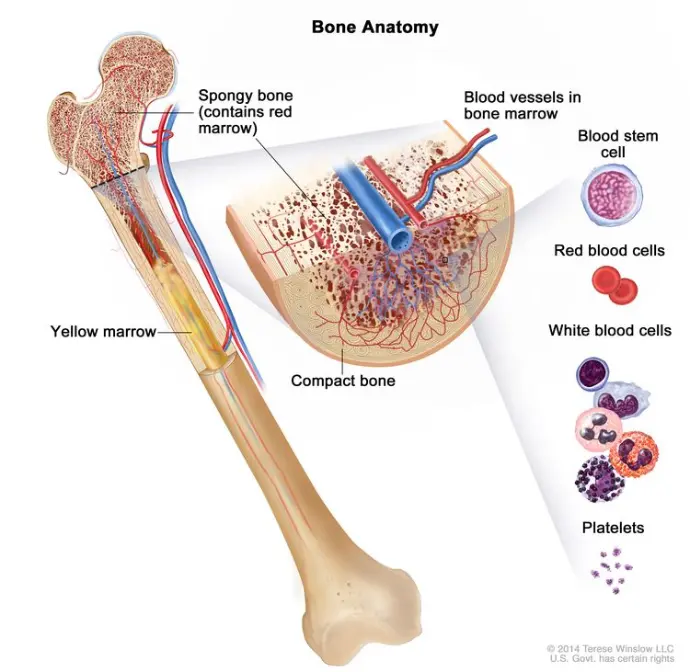
- Bone Marrow Transplant : Often used in blood cancers.
In many cases, a multidisciplinary approach combining several therapies is used to increase effectiveness.
Living with Cancer
A cancer diagnosis changes a person’s life, but support, education, and awareness make a difference. Mental health support, nutrition, physical activity, and palliative care are essential aspects of living with cancer. Survivorship and life after treatment are also important focuses of care today.